In the intricate landscape of neurology and medical science, Vagus Nerve Stimulation (VNS) emerges as a captivating frontier, offering profound insights into the modulation of nerve activity for therapeutic benefits. This comprehensive exploration seeks to unravel the mysteries surrounding VNS, delving into its anatomical foundations, medical applications, procedural intricacies, and the potential it holds for transforming treatment paradigms.
What is Vagus Nerve Stimulation (VNS)?
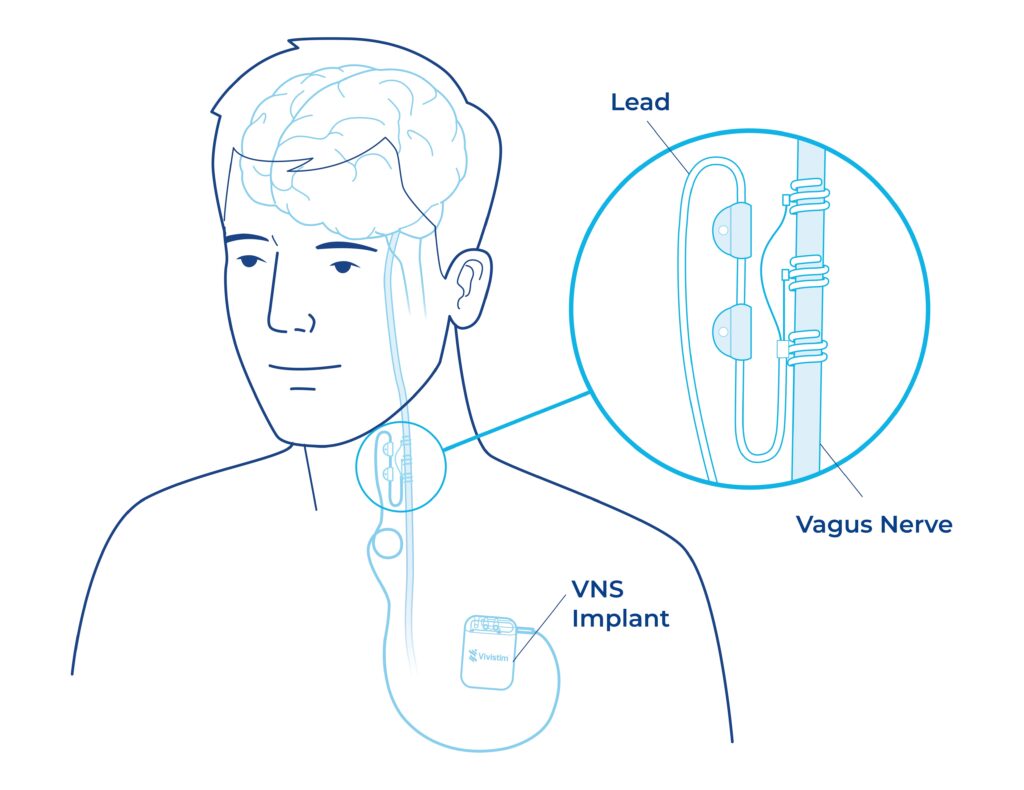
The vagus nerve, the tenth cranial nerve, intricately weaves its way from the brainstem through the neck, chest, and abdomen, influencing an array of physiological functions. Understanding the anatomy of this extensive nerve provides a crucial backdrop for comprehending the transformative effects of VNS. It acts as a communication highway, transmitting signals between the brain and vital organs, controlling functions ranging from heart rate to digestion.
Vagus Nerve Stimulation (VNS) Overview
VNS, a form of neuromodulation, stands as a beacon of innovation in the treatment landscape. It involves the implantation of a device that sends measured electrical pulses to the brainstem through the vagus nerve. Often referred to as a “pacemaker for the brain,” VNS steps into the therapeutic arena when traditional treatments prove ineffective. It has found its niche in addressing treatment-resistant epilepsy, depression, and more recently, stroke rehabilitation.
Medical Applications of VNS:
- Epilepsy Treatment: VNS serves as an adjunctive therapy for focal seizures, offering a novel approach to those resistant to conventional anticonvulsants.
- Depression and Mood Disorders: As a potential mood regulator, VNS presents a treatment avenue for individuals grappling with long-term or recurrent major depression that hasn’t responded to multiple antidepressants.
- Stroke Rehabilitation: The recent approval of VNS as a rehabilitation aid after stroke marks a significant stride, aiming to enhance motor function in those with moderate to severe limb impairment.
How does Vagus Nerve Stimulation work?
Despite its transformative effects, the precise mechanisms driving VNS-induced changes remain a scientific enigma. For epilepsy control, the focus is on improved blood flow, modification of seizure-inducing electrical patterns, and elevation of neurotransmitter levels. In depression, the alteration of neurotransmitter levels governing mood takes center stage, while in stroke rehabilitation, targeted stimulation of the motor cortex becomes pivotal.
VNS Procedure Details:
From pre-surgery preparations to the intricate device implantation process, the VNS procedure involves a meticulous series of steps. Post-surgery, device activation, and adjustment, coupled with regular follow-ups, ensure optimal functioning. The necessity of battery replacement every six years adds a layer of continuity to the treatment process.
Risks, Benefits, and Recovery:
While VNS brings promising therapeutic outcomes, it is not without its share of risks. Infections, pain, and inflammation are common, and side effects like coughing and hoarseness may be present. However, these can often be mitigated through adjustments. Serious complications, though rare, include vocal cord paralysis and cardiac arrest. Fortunately, recovery is swift, with self-absorbing stitches and a relatively short recovery period.
Are there any side effects associated with Vagus Nerve Stimulation?
Common side effects may include hoarseness, coughing, or throat discomfort. Serious side effects are rare but can include infection or changes in voice.
Outlook and Ongoing Research
The outlook for VNS is marked by ongoing research, aiming to uncover its full potential. While it doesn’t promise a cure for epilepsy or depression, studies show significant reductions in seizures and improvements in mood. In stroke rehabilitation, VNS has demonstrated positive outcomes, enhancing limb mobility and functionality.
When to Seek Medical Attention
VNS recipients should remain vigilant for signs of infection, changes in voice, or discomfort during stimulation, prompting timely medical attention. Regular check-ups ensure the device’s proper functioning, providing a proactive approach to potential complications.
How long does it take to see results from Vagus Nerve Stimulation?
The timeline for seeing results varies among individuals. Some may experience improvements shortly after activation, while others may notice changes over time.
Is Vagus Nerve Stimulation a surgical procedure?
Yes, VNS typically involves a surgical procedure to implant a device, often referred to as a “pacemaker for the brain,” that delivers controlled electrical impulses to the vagus nerve.
Can Vagus Nerve Stimulation be used in conjunction with other treatments?
Yes, VNS can be used alongside other treatments, and its compatibility with medications and therapy makes it a versatile option for managing various conditions.
Is Vagus Nerve Stimulation a one-time procedure, or does it require ongoing maintenance?
The device may need adjustments over time, and regular follow-up appointments with healthcare providers are essential for monitoring and optimizing the treatment.
Are there any lifestyle adjustments needed after undergoing Vagus Nerve Stimulation?
In most cases, individuals can resume their normal activities after recovery from the surgical procedure. However, it’s crucial to follow any guidelines provided by healthcare professionals.
Is Vagus Nerve Stimulation suitable for everyone?
VNS is generally considered for individuals who have not responded well to other treatments. However, its appropriateness is determined on a case-by-case basis by healthcare providers.
Exploring Beyond Approved Uses:
Beyond its FDA-approved applications, VNS tantalizingly ventures into uncharted territories. Ongoing research investigates its potential in addressing inflammatory disorders, migraines, fibromyalgia, obesity, bipolar disorder, and even neurodegenerative conditions like Alzheimer’s disease.
Insurance Coverage and External Devices
Navigating the realms of insurance coverage, especially for VNS devices, requires a nuanced understanding of the specific criteria set by providers. While external VNS devices exist, their precision pales in comparison to the implanted counterparts, emphasizing the unique advantages of the latter.
Conclusion
Vagus Nerve Stimulation stands at the forefront of medical innovation, weaving a narrative of hope and transformation for individuals facing treatment-resistant conditions. As the mysteries surrounding its mechanisms unfold and research paves the way for expanded applications, VNS emerges as a beacon of promise, illuminating the path toward a future where neurological disorders are met with novel, effective, and personalized interventions.